UDA Training: Insulin Basics
Diabetes Aide TrainingComplete all of the following modules:
As you complete this training course the RN responsible for delegating the task of insulin administration should be available to discuss the content and answer your questions.
Insulin Basics
Insulin is a hormone that is produced in the body’s pancreas. Insulin moves glucose (sugar) from the blood into the cells for energy. People with type 1 diabetes do not produce insulin anymore. People with type 2 diabetes produce insulin, but the amount is not enough, and the body does not use the insulin properly. Without enough insulin, high blood glucose levels result; this can be a serious and life-threatening situation.
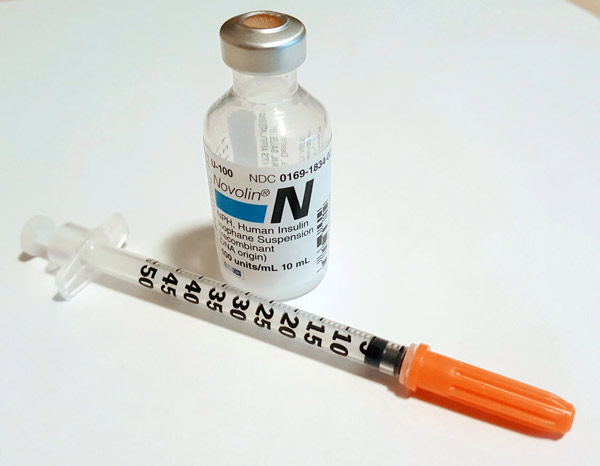
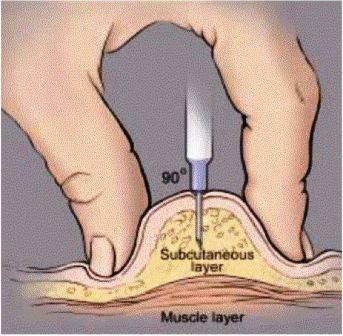
Insulin is administered subcutaneously
Subcutaneous (SQ) injections administer medications into the fatty layer of tissue just under the skin. Insulin is administered subcutaneously by one of three ways as shown in the pictures below.
- Vial and syringe
- Insulin Pen
- Insulin Pump
Methods of insulin administration will be covered in more detail in Module 6.
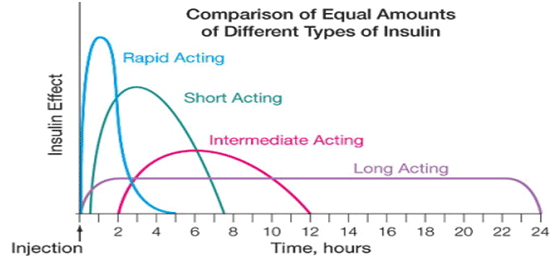
Types of Insulin
More than one type of insulin is available. Doctors prescribe the type and amount of insulin according to a person’s specific needs. Types of insulin fall into these categories:
- rapid-acting
- short-acting
- intermediate-acting
- long-acting
- pre-mixed
"Insulin action" is when a type of insulin begins working, when it is most active and how long it keeps working. Insulin action will vary from person to person. It will even vary from day to day in the same person depending on the activities of the person and the insulin injection site. A comparison of different types of insulin is shown in the graph. Please remember that people respond uniquely to the different insulin types so the graph should be used only as a guide.
Rapid-acting
Rapid-acting insulin starts working quickly, in about 5-15 minutes, has a peak effect in 30-90 minutes, and quits working in about 5 hours. It is given immediately before or right after meals and is administered by vial and syringe, insulin pen, or by insulin pumps.
- Apidra (glulisine)
- Humalog (lispro)
- NovoLog (aspart)
Short-acting
Short-acting insulin, called Regular or “R” begins to act about 30-60 minutes after it is given, has a peak effect 2–4 hours after injection, and lasts about 6-9 hours.
Intermediate-acting
Intermediate-acting insulin, NPH or “N”, absorbs more slowly into the body and lasts longer, has its peak activity 4-8 hours after injection and lasts about 13 hours for most people. When NPH is taken in the morning for instance it may peak before supper.
Long-acting
Long-acting insulin, Lantus and Levemir, has almost no peak activity and lasts between 20-24 hours for most people.
Pre-mixed
Pre-mixed insulins are a mixture of rapid/short-acting insulin and intermediate-acting insulin. An advantage of taking pre-mixed insulin is that people do not need to have two different types of insulins.
- Humulin 70/30
- Humalog Mix 75/25
- Humalog Mix 50/50
- NovoLog Mix 70/30
Insulin Storage
- The vial or pen currently used for a patient/student should be kept at room temperature.
- Extra vials and pens should be stored in the refrigerator.
- Make certain the insulin does not freeze or get too warm (above 86 degrees). If the insulin does freeze or get too warm it may not be effective and should be discarded.
- Always check the expiration date on the insulin bottle (vial) or pen. Outdated insulin bottles and pens should be discarded.
- After gently rolling the vial, if there are signs of yellowing or clumping in the vial, discard the vial.
- Know how long a vial/pen can be used once it’s opened. This varies by type of insulin, so check with the RN for the information.
Insulin Dosing
Insulin is measured in units. The number of insulin units the person with diabetes is to receive will be ordered by their physician. The physician’s order will be part of the Diabetes Medical Management Plan for school children or for other persons the order may be listed on a medication administration record (MAR). Make sure you and the RN discuss the medication order sheet your facility uses.
The doctor may order insulin doses to be administered in three ways:
1. Fixed dose (or Set amount)
Fixed dose (or Set amount): When the physician orders a fixed dose of insulin, the person with diabetes will get the same amount at the same time every day.
- Example: Give 5 units R insulin at 8 a.m. each day.
- Example: NovoLog 4 units at breakfast, 5 units at lunch, 5 units at supper.
- Example: Lantus 10 units at bedtime.
2. Sliding Scale
Sliding Scale orders mean the person with diabetes will be administered a dose of insulin (or extra units of insulin) based on the results of their blood glucose test. This is called a sliding scale order because the person’s dose of insulin units to be administered will ‘slide’ up or down depending on his or her blood sugar results. The physician orders a different amount of insulin to be administered based on the person’s blood glucose level.
Usually one of the following types of rapid-acting insulin is ordered by the physician for the sliding scale order: Apidra, Humalog or NovoLog, or a short-acting insulin,
such as Regular insulin. Sliding scale insulin is usually given at meal times, but may also be given at other times to bring down a high glucose level.
When a person is getting sliding scale insulin, the blood glucose level needs to be checked first in order to determine how much insulin to give.
Sometimes sliding scale insulin is given alone, and sometimes it is added to a fixed dose of insulin at meal times. Discuss with the RN to make certain
you understand and give the correct dose of insulin using a sliding scale.
Examples of sliding scale orders.
Physician order for John:
| Blood Sugar Results(mg/dl) | Administer Regular Insulin |
|---|---|
| Below 70 = | Follow protocol for hypoglycemia (notify RN) |
| 71-200 | No sliding scale insulin needed |
| 201-250 | 4 units SQ |
| 251-300 | 6 units SQ |
| 301-350 | 8 units SQ |
| Above 350 | Follow hyperglycemic protocol (notify RN) |
Practice using the sliding scale above.
- On Monday, John’s blood sugar at 9 a.m. is 210 mg/dl. How many units of insulin should you administer? (Answer: 4 units of Regular insulin SQ)
- Later that day, at 5 p.m., his blood sugar is 312 mg/dl. How many units of insulin should you administer? (Answer: 8 units of Regular insulin SQ)
- On Tuesday, at 9 a.m. John’s blood sugar is 188 mg/dl. How many units of insulin should you administer? (Answer: he will not receive any sliding scale insulin because he only gets additional sliding scale insulin for blood sugars over 200 mg/dl.)
- Later that day, at 5 p.m., his blood sugar is 300 mg/dl. How many units of insulin should you administer? (Answer: 6 units of Regular insulin SQ)
Physician order for Mary:
| Blood Glucose Level | NovoLog units |
|---|---|
| Under 150 | 0 |
| 150-200 | 2 |
| 201-250 | 4 |
| 251-300 | 6 |
| 301-350 | 8 |
| Over 350 | Notify RN to contact physician |
Practice using the sliding scale above.
- Before breakfast on Saturday, Mary’s blood sugar is 192 mg/dl. How many units of Novolog insulin should you administer? (Answer: 2 units)
- You check Mary’s blood sugar before lunch and it is 362 mg/dl. How many units of insulin should you administer? (Answer: Call the delegating RN. The RN will notify the physician to obtain additional orders.)
- Before supper Mary’s blood sugar is 266 mg/dl. How many units of Novolog insulin should you administer? (Answer: 6 units)
3. Insulin-to-carbohydrate ratio
Insulin-to-carbohydrate ratio is used to give insulin based on the amount of carbohydrate a person eats at a meal. This method provides more flexibility with meal planning and may help keep a person’s blood glucose levels more “tightly controlled” or to stay within the recommended blood glucose range.
An example of an insulin-to-carbohydrate ratio order a physician may write is, “Administer 1 unit of Novolog insulin for every 15 grams of carbohydrate eaten”; this is a 1:15 insulin to carbohydrate ratio. The total carbohydrate grams eaten are divided by 15 to determine the number of insulin units that need to be administered. An example of a meal eaten by a person with diabetes that takes insulin according to insulin to carb ratio of 1:15.
| Food | Carbohydrate Grams | |
|---|---|---|
| Turkey sandwich on 2 slices of wheat bread | 30 | |
| Carrots with Ranch dip | 0 | |
| Small orange | 15 | |
| Diet soda | 0 | |
| TOTAL GRAMS = | 45 | |
| Total grams of carbs eaten | Carb Ratio is 1:15 | Insulin units |
| 45 | ÷ 15 grams = | 3 units |
The person needs 3 units of insulin administered, this is their "meal" insulin dose.
Correction Factor Dose
In addition to the “meal” insulin dose, a physician may also order a correction factor dose to be administered at the same time. Sometimes this is also referred to as a “sensitivity” dose. The reason a physician orders a correction dose is to bring down a high blood glucose level at a meal. If the current blood glucose before the meal is at or below the target blood glucose level, you do not need to give any correction insulin for that meal.
To figure out the correction dose three things must be considered:
- Current blood glucose level (example: 350)
- Target blood glucose level (example: 150)
- Sensitivity – the number of points that 1 unit of rapid-acting insulin should drop the blood glucose (example: 50; one unit of insulin should drop the blood sugar by 50 points)
Example of a physician order for a correction factor.
| Correction factor: blood glucose level minus 150 divided by 50 | |
|---|---|
| 350 | |
| 350-150=200 | |
| 200/50=4 | |
| Correction factor insulin dose is 4 units | |
Rounding Numbers
In the example above, the number of units equaled whole numbers, 3 and 4 units. But often the number of units will not be a whole number and instead will be a number like 4.3 for instance. When the dose is not a whole number you will need to round the number to a whole number. Guidelines for rounding are as follows:
- Do not round until you have calculated the TOTAL insulin dose (both the "meal" and the "correction factor" doses).
- If the person is administered whole unit doses of insulin, round to the nearest whole number.
- If the person gets half unit doses, round to the nearest half number.
Practice: Whole Unit Administration
Henry's physician has ordered the following insulin to be administered. His current blood glucose level is 412.
| Administer NovoLog insulin after meals using an insulin to carb ratio of 1 unit for every 15 grams of carbs eaten. Use a correction factor for a blood glucose target of 150 and a sensitivity of 50. | |
| Henry eats the following meal: | |
| Food: | Carbohydrate Grams: |
| Chicken breast, no breading | + 0 |
| ½ cup Green beans | + 0 |
| ½ cup mashed potatoes | + 15 |
| ¼ cup gravy | + 0 |
| 1 dinner roll | + 30 |
| ½ cup skim milk | + 15 |
| TOTAL Number of carb grams eaten? | = |
| Carb Ratio: | ÷ 15 grams |
| Number of units of insulin to administer for “meal” insulin dose: | = units |
Correction Factor: |
|
| Current blood glucose level | ? |
| Subtract target blood glucose level |
-
= |
| Divide by the Sensitivity: | ÷ |
| Number of units of insulin to administer for “correction factor” insulin dose: | = units |
| Add “meal” insulin dose: | + units |
| TOTAL number of units of insulin: | = total |
| Round number if needed to determine TOTAL insulin dose to administer: | ~ units |
Whole Unit Administration Table
| Number you get | Round to |
|---|---|
| 0-1.4 | 1 unit |
| 1.5-2.4 | 2 units |
| 2.5-3.4 | 3 units |
| 3.5-4.4 | 4 units |
| 4.5-5.4 | 5 units |
| 5.5-6.4 | 6 units |
| 6.5-7.4 | 7 units |
| 7.5-8.4 | 8 units |
| 8.5-9.4 | 9 units |
| 9.5-10.4 | 10 units |
Answer
Henry ate 60 grams of carbohydrate, so 4 units of insulin should be administered for his "meal" dose. For his "correction factor" dose, his blood sugar was 412. Subtract target blood glucose of 150 from his current blood sugar of 412 to equal 262. Divide 262 by sensitivity factor of 50 to equal 5.24. Add the "meal" dose of 4 units to the "correction factor" dose of 5.24 to equal 9.24. Round this number to get your TOTAL insulin dose of 9 units.
Practice: Half Unit Administration
Megan's physician has ordered the following insulin to be administered. Her current blood glucose level is 224.
| Administer NovoLog insulin after meals using insulin to carb ratio of 1 unit of insulin for every 60 grams of carbs eaten. Use a correction factor for a blood glucose target of 150 and a sensitivity of 120. | |
| Megan eats the following meal: | |
| Food: | Carbohydrate Grams: |
| 3/4 cup of Cheerios | + 15 |
| 1 cup milk | + 15 |
| 1 slice of toast | + 15 |
| 1 egg | + 0 |
| 2 slices of bacon | + 0 |
| TOTAL Number of carb grams eaten? | = |
| Carb Ratio: | ÷ 60 grams |
| Number of units of insulin to administer for “meal” insulin dose: | = units |
Correction Factor: |
|
| Current blood glucose level | ? |
| Subtract target blood glucose level |
-
= |
| Divide by the Sensitivity: | ÷ |
| Number of units of insulin to administer for “correction factor” insulin dose: | = units |
| Add “meal” insulin dose: | + units |
| TOTAL number of units of insulin: | = total |
| Round number if needed to determine TOTAL insulin dose to administer: | ~ units |
Whole Unit Administration Table
| Number you get | Round to |
|---|---|
| 0-1.4 | 1 unit |
| 1.5-2.4 | 2 units |
| 2.5-3.4 | 3 units |
| 3.5-4.4 | 4 units |
| 4.5-5.4 | 5 units |
| 5.5-6.4 | 6 units |
| 6.5-7.4 | 7 units |
| 7.5-8.4 | 8 units |
| 8.5-9.4 | 9 units |
| 9.5-10.4 | 10 units |
Half Unit Administration Table
| Number you get | Round to |
|---|---|
| 0-0.74 | 1/2 unit |
| 0.75-1.24 | 1 unit |
| 1.25-1.74 | 1 1/2 units |
| 1.75-2.24 | 2 units |
| 2.25-2.74 | 2 1/2 units |
| 2.75-3.24 | 3 units |
| 3.25-3.74 | 3 1/2 units |
| 3.75-4.24 | 4 units |
| 4.25-4.74 | 4 1/2 units |
| 4.75-5.24 | 5 units |
Answer
Megan ate 45 grams of carbohydrate, so 0.75 unit of insulin should be administered for her "meal" dose. For her "correction factor" dose, her blood sugar was 224. Subtract target blood glucose of 150 from current blood glucose of 224 to equal 74. Divide 74 by sensitivity factor of 120 to equal 0.61. Add the "meal" dose of 0.75 unit to the "correction factor" dose of 0.61 unit = 1.36. Round this number to get your TOTAL insulin dose of 1 "whole" unit or 1 ½ "half" units of insulin.




.jpg)