UDA Training: Blood Glucose Monitoring
Diabetes Aide TrainingComplete all of the following modules:
As you complete this training course the RN responsible for delegating the task of insulin administration should be available to discuss the content and answer your questions.
Blood Glucose Monitoring
Blood glucose monitoring, is an important part of diabetes care. Sometimes people refer to this blood test as a "blood sugar".
This blood test helps the person’s doctor (or other health care provider) identify trends for high and low blood sugars. Accurate blood glucose monitoring is important. The doctor determines the appropriate insulin doses and treatment changes based on blood glucose monitoring.
Terminology
Terms you need to know.
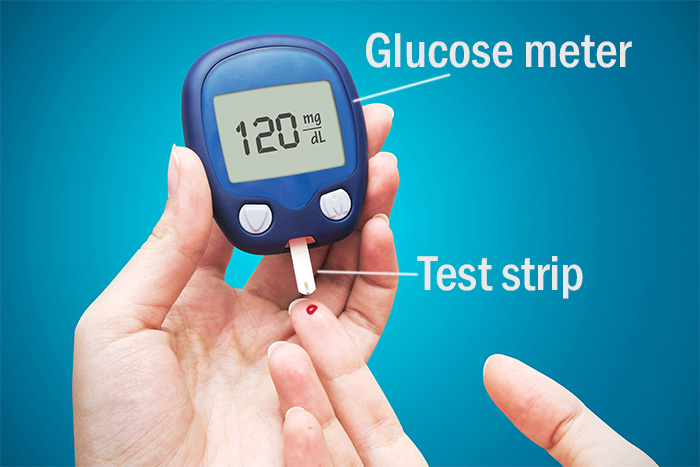
Glucose meter
Glucose meter: a machine used for testing the amount of glucose (sugar) in the blood. There are a variety of blood glucose meters available for use. Glucose meters are generally small, easy to use, and reliable. You will need to know how to use the machine for the person you will help.
Test strips
Test strips: strips with chemicals (reagents) on them that react with the glucose in the blood. Each test strip is used only one time and then should be discarded appropriately.
Coding
Coding: some meters require a code number or chip be placed into the meter; the code corresponds to the test strips. If the code is not correct, the glucose result will not be accurate. Consult with your delegating RN to help you with coding the meter if necessary.
Lancet
Lancet: a small needle used to poke the finger to obtain a blood sample. You might use a lancet that came with a meter or you might use a lancet provided by your facility. Lancets should only be used once. NEVER use the same lancet on more than one patient. Lancets should be disposed of in a sharps container.
Lancing Device
Lancing Device: lancets are either self-contained or are placed in a lancing device. Most lancing devices can be adjusted for depth so that an adequate amount of blood can be obtained with maximum comfort. NEVER use the same lancing device on more than one person!
When should a person’s blood glucose be tested?
Usually the person’s doctor/health care provider will decide how often the blood glucose should be checked. Blood glucose tests are generally monitored and performed:
- Before meals
- One to two hours after meals, and
- Before bedtime
Extra blood glucose testing may also be needed, such as when a person shows symptoms of hypoglycemia
low blood sugar) or when the person has been doing lots of physical activity.
A person’s blood glucose levels vary throughout the day. It is important to know the "target" blood
sugar for the time of day you are testing. The doctor generally includes a person’s "target" blood
glucose range in the person’s medical orders. Once you have the results of a blood glucose test you
need to look at the target range and follow the directions in the patient’s medical orders or the
student’s Diabetes Medical Management Plan (DMMP) accordingly.
It is important that you discuss with your delegating RN the times that a person's
blood glucose needs to be checked.
Some people with diabetes test their own blood sugar. It is important to let the
person with diabetes help with the testing whenever possible. The RN may assess
the patient/student to identify if a person is capable of doing the test themselves
or to identify what level of help the person needs. The nurse will determine whether
or not a person can perform the test independently depending on the person’s:
- Dexterity: for example, the person must be able to use their fingers to do the test;
- Cognition: for example, the person must be able to remember the steps to do the test;
- Problem solving ability: for example, the person must be able to recognize and trouble shoot problems, such as if they have too much or too little blood on the test strip.
Pay attention to the following things that can affect the accuracy of the glucose test. Try to avoid the following:
- Operator error – such as not cleaning the finger correctly
- Inappropriate sample size – such as too small a sample of blood on the strip
- Inaccurate meter code
- Expired strips – expired strips should be discarded
Discuss issues affecting the accuracy of the testing with your delegating RN.
Blood Glucose Testing
- Wash hands
- Gather supplies:
- Glucose meter
- Test strips
- Lancing device and lancet
- Gloves
- Cotton balls
- Alcohol wipes
- Check the expiration on the test strips
- Put on gloves
- Prepare the lancing device
- Insert the strip and turn on the meter
- Check the code (if necessary)
- Cleanse skin appropriately with alcohol wipe or soap and water
- Lance the finger in appropriate area
- Obtain a blood sample
- Apply blood to test strip
- Place cotton ball or tissue over lanced area
- Read the result and record appropriately
- Turn meter off /remove strip
- Dispose of all supplies as appropriate
- Wash hands
Locations to lance fingers:
Watch the video demonstrating the steps for performing blood glucose monitoring. The video will help you prepare to practice and safely perform this task with your delegating RN.
The red dots on the fingers indicate the locations to poke the fingertips.